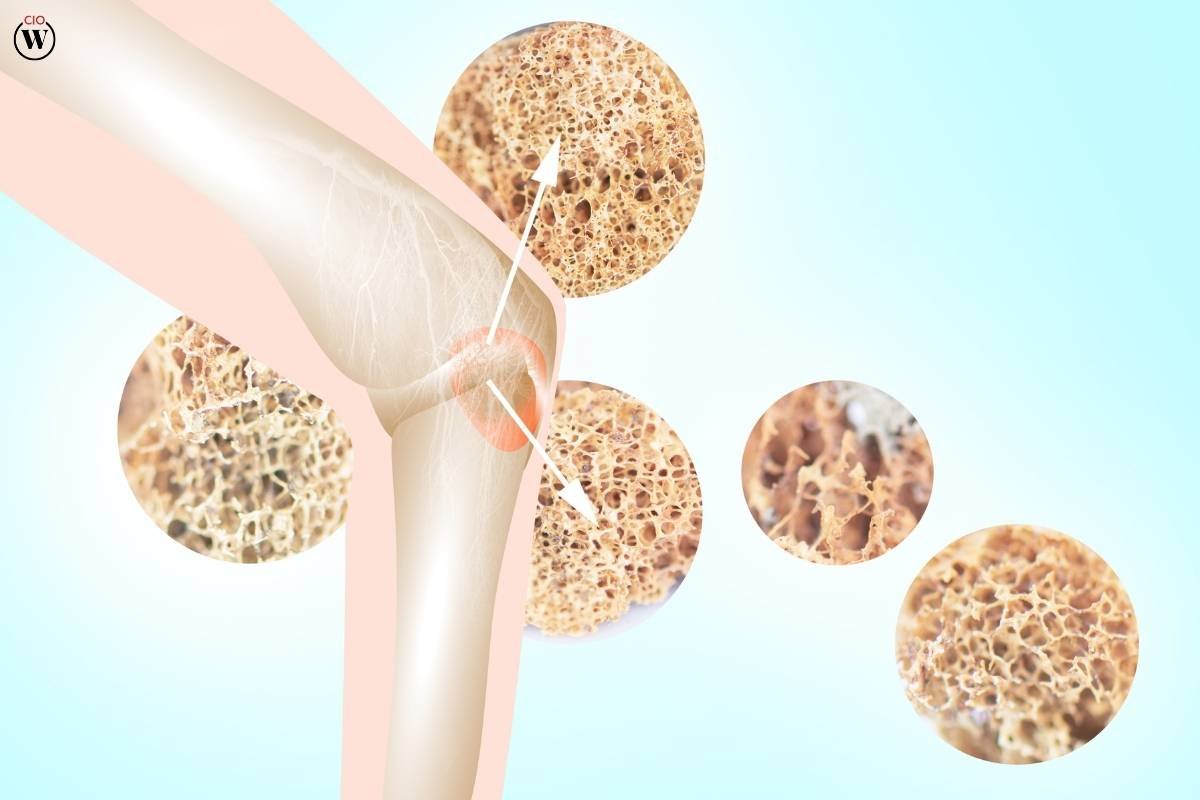
Osteoporosis is a prevalent condition characterized by weakened bones, making them more susceptible to fractures. Affecting millions of people worldwide, this condition particularly targets postmenopausal women, though men are also at risk. In the quest to manage and treat osteoporosis, the development and administration of effective drugs have become paramount. This article delves into the various types of drugs for osteoporosis, their mechanisms, and their impact on patients’ lives.
Understanding Osteoporosis
Osteoporosis translates to “porous bone.” It occurs when the creation of new bone doesn’t keep up with the removal of old bone. This imbalance leads to bones becoming brittle and fragile. Factors such as age, gender, hormonal changes, and lifestyle choices contribute to the development of osteoporosis. The primary goal in treating osteoporosis is to prevent fractures, which can significantly impair quality of life and increase mortality rates, particularly in the elderly.
Types of Drugs for Osteoporosis
There are several categories of drugs for osteoporosis, each working through different mechanisms to maintain or improve bone density.
1. Bisphosphonates
Bisphosphonates are the most commonly prescribed drugs for osteoporosis. They work by inhibiting the activity of osteoclasts, the cells responsible for bone resorption. By reducing bone breakdown, these drugs help maintain bone density. Common bisphosphonates include:
- Alendronate (Fosamax)
- Risedronate (Actonel)
- Ibandronate (Boniva)
- Zoledronic acid (Reclast)
2. Selective Estrogen Receptor Modulators (SERMs)
SERMs mimic the beneficial effects of estrogen on bone density without some of the risks associated with estrogen therapy. Raloxifene (Evista) is a well-known SERM used as a drug for osteoporosis. It helps reduce the risk of spinal fractures in postmenopausal women.
3. Parathyroid Hormone Analogues
Teriparatide (Forteo) and abaloparatide (Tymlos) are synthetic forms of parathyroid hormone. Unlike other treatments that slow down bone loss, these drugs for osteoporosis stimulate new bone growth. They are typically used for patients with severe osteoporosis or those who haven’t responded well to other treatments.
4. RANK Ligand (RANKL) Inhibitors
Denosumab (Prolia) is a RANKL inhibitor that works by targeting and inhibiting the activity of osteoclasts. Administered via injection every six months, this drug for osteoporosis has shown efficacy in reducing the risk of fractures in various bones.
5. Calcitonin
Calcitonin is a hormone involved in calcium regulation and bone metabolism. Available as a nasal spray or injection, calcitonin (Miacalcin) is used less frequently today due to the availability of more effective treatments. However, it can be beneficial for patients who cannot tolerate other drugs for osteoporosis.
6. Romosozumab
Romosozumab (Evenity) is a newer option that both increases bone formation and decreases bone resorption. It is administered as a monthly injection and is usually prescribed for postmenopausal women at high risk of fractures.
Mechanisms of Action
Understanding how these drugs for osteoporosis work helps in comprehending their role in bone health management.
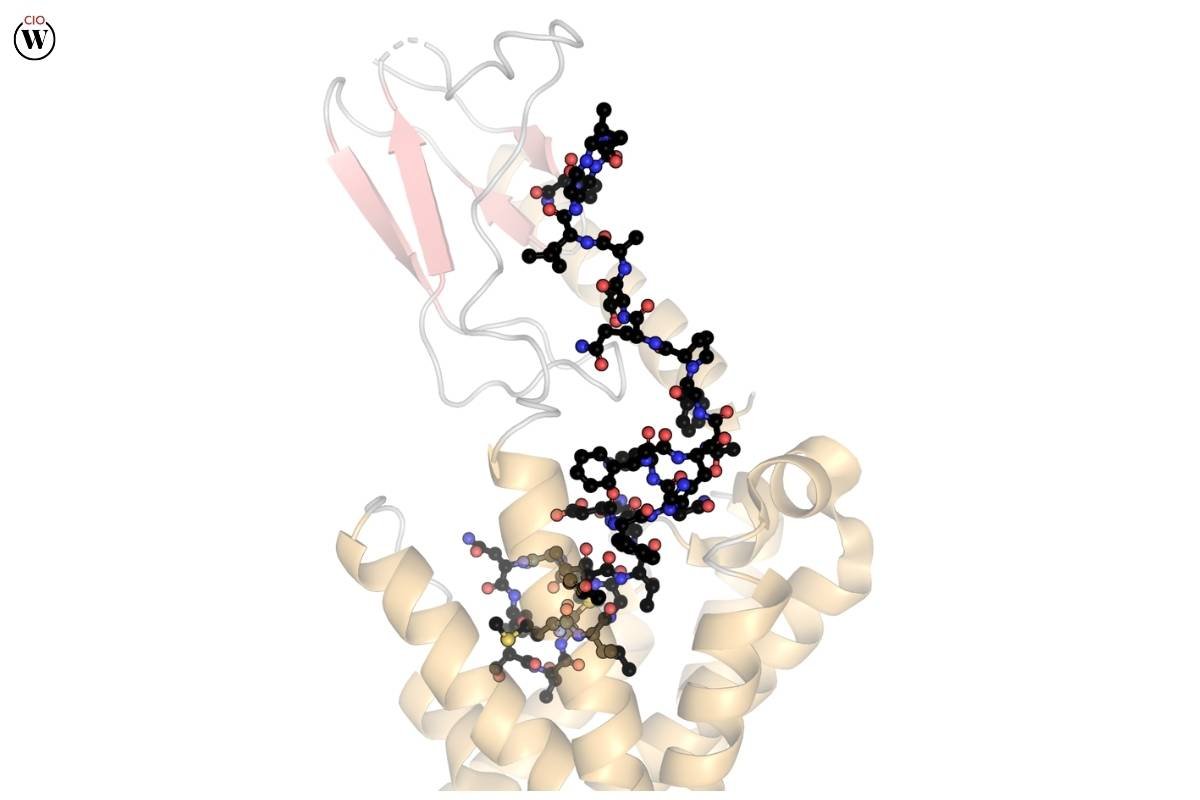
- Bisphosphonates: They attach to bone minerals and inhibit osteoclast-mediated bone resorption, which slows down the overall process of bone loss.
- SERMs: By selectively activating estrogen receptors in bone tissue, SERMs help maintain bone density and reduce the risk of fractures.
- Parathyroid Hormone Analogues: These drugs stimulate bone formation by acting on bone-building cells called osteoblasts.
- RANKL Inhibitors: By blocking the interaction between RANKL and its receptor on osteoclasts, these inhibitors reduce the formation and activity of osteoclasts, leading to decreased bone resorption.
- Calcitonin: It directly inhibits osteoclast activity and can also promote the excretion of calcium through the kidneys.
- Romosozumab: This drug has a dual effect; it both promotes the activity of osteoblasts (bone-building cells) and inhibits the activity of osteoclasts.
Efficacy and Safety
The efficacy of drugs for osteoporosis is often measured by their ability to increase bone mineral density (BMD) and reduce the risk of fractures. Bisphosphonates, for instance, have been shown to significantly reduce the risk of hip, spine, and other fractures. SERMs like raloxifene are effective in reducing the risk of vertebral fractures but less so for non-vertebral fractures.
Parathyroid hormone analogues and RANKL inhibitors also demonstrate substantial efficacy in improving BMD and reducing fracture risk. However, these treatments often come with considerations regarding long-term safety. For instance, prolonged use of bisphosphonates has been associated with rare but serious side effects like osteonecrosis of the jaw and atypical femoral fractures.
Side Effects and Considerations
Every drug for osteoporosis comes with potential side effects. Common side effects of bisphosphonates include gastrointestinal issues, such as esophageal irritation and ulcers. SERMs may increase the risk of blood clots, which is a significant consideration for patients with a history of cardiovascular issues.
Parathyroid hormone analogues can cause hypercalcemia (high calcium levels) and have a black box warning for potential osteosarcoma (a type of bone cancer). Denosumab has been associated with infections and dermatologic reactions due to its immune-modulating effects.
Given these considerations, it’s crucial for healthcare providers to tailor osteoporosis treatment to each patient’s specific risk profile and medical history. Regular monitoring and follow-up are essential to manage any adverse effects and ensure the optimal benefit of the treatment.
Emerging Therapies
Research in the field of osteoporosis is ongoing, with new potential treatments on the horizon. An exciting area of development is the use of sclerostin inhibitors. Sclerostin is a protein that inhibits bone formation; thus, blocking its action can promote bone growth. Romosozumab is the first drug in this class, showing promise in clinical trials and offering hope for even more effective management of osteoporosis in the future.
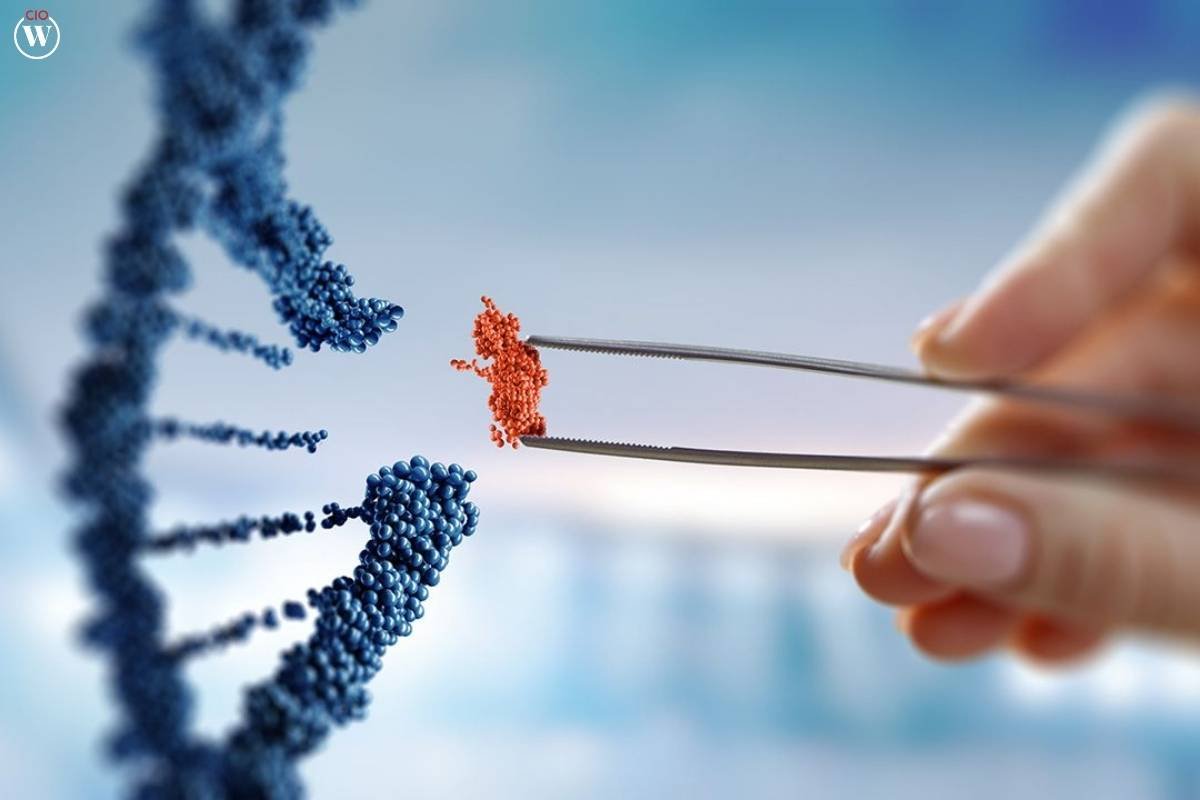
Additionally, gene therapy and stem cell research are being explored as potential avenues for treating osteoporosis. While these therapies are still in the experimental stages, they hold significant potential for revolutionizing the approach to managing bone health.
Lifestyle and Non-Pharmacological Interventions
While discussing drugs for osteoporosis, it is also important to acknowledge the role of lifestyle and non-pharmacological interventions. Adequate intake of calcium and vitamin D is essential for bone health. Weight-bearing exercises, such as walking, jogging, and strength training, can help maintain bone density and strength.
Smoking cessation and moderation of alcohol intake are also crucial, as these factors can exacerbate bone loss. Fall prevention strategies, including home safety assessments and balance training, can significantly reduce the risk of fractures in individuals with osteoporosis.
Conclusion
Osteoporosis is a condition that requires a multifaceted approach for effective management. The development of various drugs for osteoporosis has significantly improved the outlook for individuals at risk of fractures due to this condition. From bisphosphonates to newer options like romosozumab, these medications offer diverse mechanisms of action tailored to different patient needs.
However, it’s vital for patients and healthcare providers to weigh the benefits and risks of each drug for osteoporosis, considering potential side effects and individual patient profiles. Ongoing research and emerging therapies continue to enhance the arsenal against osteoporosis, promising even better outcomes in the future.
In conclusion, the management of osteoporosis is a dynamic field, with drugs for osteoporosis playing a central role in preserving bone health and preventing fractures. Alongside pharmacological treatments, lifestyle modifications and preventive measures remain integral to a comprehensive approach to bone health. As the understanding of osteoporosis evolves, so too does the potential for more effective and safer treatments, offering hope to those affected by this debilitating condition.









